Global Healthcare Markets eXpo
Find Healthcare Professionals in Your Community
We Help Patients Find Health Care Providers and Health Industry Professionals Find Business Partners.
We provide patients and health affiliates the tools to thoroughly find care and do business with the right professionals through our exposition-style directory.

Physicians & Surgeons

Clinics & Polyclinics

Hospitals

Dentists / Dental Care

Health & Wellness

Manufacturers & Supply Chain Management
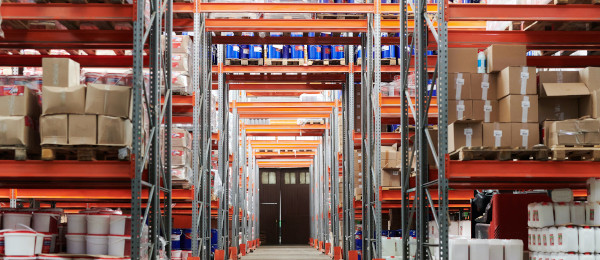
Distributors & Supply Chain Operations

Corporate Sponsors & Strategic Partners


